When a tooth has been missing for a while, the jawbone in that area can gradually thin. Dental implants need healthy, stable bone for long-term support, so some people benefit from bone grafting before an implant is placed. If you are comparing options for dental implants in Toronto or planning a consultation, understanding how grafting works will help you feel prepared and confident.
Why bone grafting is sometimes needed
Teeth stimulate the jaw when you chew. Without that stimulation, the bone can shrink in width and height. Gum disease, long-standing tooth loss, and certain medical conditions can speed up this change. Bone grafting adds volume and density where the implant will go, creating a foundation that can handle everyday bite forces.
Not everyone needs a graft. If a tooth was removed recently and the surrounding bone is thick and healthy, an implant may be placed without additional procedures. If the area is thin or the upper back jaw is close to the sinus, a graft can reduce risks and improve the likelihood of strong integration.
The materials dentists use
Several safe, well-studied graft materials are available. Your dentist will recommend one or a combination based on your goals and anatomy.
- Autograft: bone taken from another area of your body. This has excellent healing potential but is used less often today because it requires a second surgical site.
- Allograft: processed human donor bone. It is widely used and carefully screened.
- Xenograft: processed bone from nonhuman sources, often bovine. It acts as a long-lasting scaffold that your body gradually replaces.
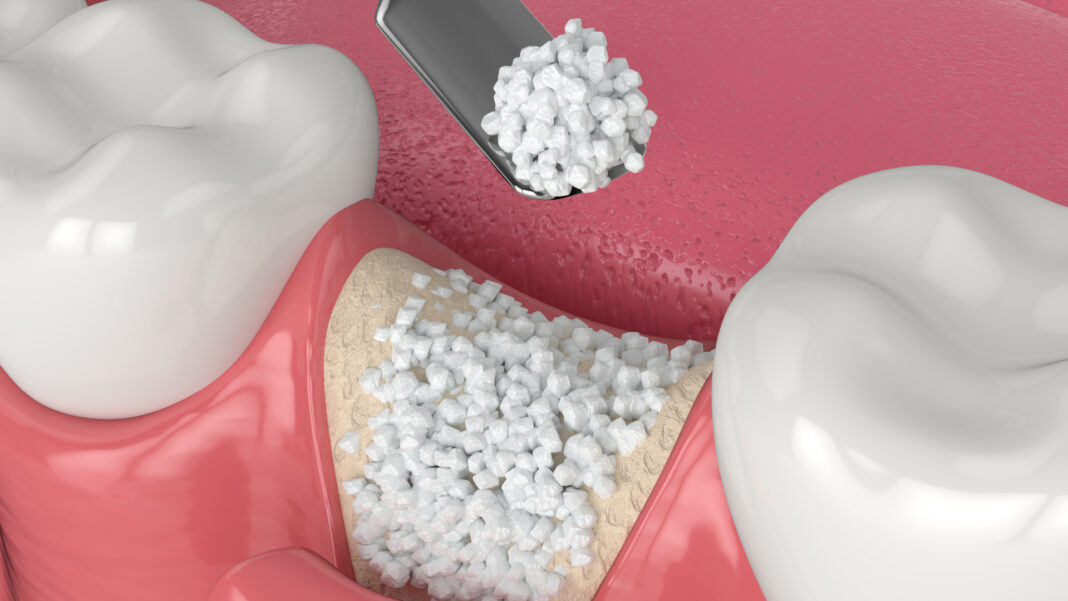
- Alloplast: synthetic options such as calcium phosphate granules that support new bone growth.
Each material is designed to be biocompatible. Some encourage the body to remodel quickly, while others maintain space over a longer time so your natural bone can fill in at a steady pace.
Common grafting procedures before implants
Socket preservation at the time of extraction
Right after a tooth is removed, the dentist can place graft material directly into the socket and secure it with a small membrane. This helps maintain the ridge shape so an implant can be planned later with less additional work.
Ridge augmentation
If the ridge has already thinned, the dentist places graft material along the narrow area and may use a small barrier membrane to protect it while it heals. This restores width and sometimes height so the implant can be positioned correctly.
Sinus lift
In the upper back jaw, the sinus can sit close to the roots. When the bone height is limited, a sinus lift gently raises the sinus floor and places graft material beneath it. This creates the vertical space needed for a stable implant.
What the step-by-step process looks like
- Evaluation and planning
A dentist will review your medical history and take imaging. Many practices use 3D scans to measure bone thickness, map nerves, and plan the exact implant location.
- Graft placement
During a brief procedure, the area is numbed. The dentist places the graft material, shapes it, and often covers it with a thin membrane. Stitches secure the site. Most people describe mild to moderate soreness for a day or two.
- Healing
Your body replaces the graft with new bone over several months. Small grafts, such as socket preservation, may be ready for implants in three to four months. Larger ridge augmentations or sinus lifts can take four to six months or longer, depending on health, smoking status, and the exact technique.
- Implant placement
Once healing is confirmed, the implant is placed into the new, stronger foundation. The implant then integrates with the bone. After that, the abutment and crown complete the restoration.
For a concise overview of timing and whether you may be a good candidate, Dr. Paul Branco, DDS, in Toronto, explains common questions about dental implants on his dental practice’s website.
Comfort, recovery, and at-home care
Mild swelling and tenderness are typical during the first 48 hours. Cold compresses, rest, and over-the-counter pain relief as directed help most people stay comfortable. Your dentist may prescribe an antimicrobial rinse to keep the area clean. Eat softer foods at first, keep a normal brushing routine away from the surgical site, and follow any instructions about avoiding straws and smoking.
Stitches are often removed after one to two weeks. Most people return to desk work within a day or two, although heavy lifting is best postponed until your dentist gives the okay. If a membrane was used, your dentist will monitor it and let you know when regular flossing and water flossers can be reintroduced near the area.
How dentists decide if grafting is necessary
- Bone measurements from imaging determine whether the width and height meet the threshold for implant size and stability.
- Gum health is assessed, since active periodontal disease must be treated before placing a graft or implant.
- Bite forces and grinding habits are considered, because stronger forces may require a wider implant or additional bone support.
- Systemic health factors, such as diabetes control or medications that affect bone, are reviewed to plan timing and follow-up.
If your anatomy already meets the requirements, you may be able to skip grafting. If not, the plan will outline the amount of bone needed and the estimated healing time before the implant stage.
Risks and how to lower them
Bone grafting has a high success rate. As with any surgical procedure, there are potential risks that include infection, graft material exposure, or slower healing. You can reduce these risks by keeping the area clean as instructed, avoiding tobacco and nicotine, managing health conditions closely with your physician, and attending all follow-up visits.
Call your dentist if you notice increasing pain after the third day, persistent bleeding, a fever, or a foul taste that does not rinse away. Early attention helps keep small concerns from becoming larger problems.
Alternatives when grafting is not ideal
Your dentist may sometimes recommend different approaches depending on anatomy and goals.
- Short or narrow implants for specific sites where bone height is limited
- Angled implants in full-arch plans to avoid anatomical structures
- Orthodontic tooth movement to improve spacing for a more favourable implant position
These alternatives are not for everyone, but they show how planning can be tailored when grafting is not the best fit.
What this means for your implant timeline
Grafting adds time to the overall plan, yet it often saves time and complications in the long run. A strong foundation supports reliable integration and reduces the need for adjustments later. If you are evaluating dental implants, your dentist will walk you through a personalized schedule that includes healing periods and the number of visits expected from start to finish.
Bone grafting is a predictable way to prepare thin or soft areas of the jaw for implants. With careful imaging, thoughtful material selection, and clear home-care instructions, most patients find the process straightforward. If you are weighing options with a Dentist, ask about your bone measurements, whether socket preservation is appropriate after extraction, and the expected healing time before implant placement. A tailored plan helps ensure your future implant is comfortable, functional, and built on a foundation that lasts.